San Francisco: We're OK, Really
- Marco Annunziata
- Jun 28, 2020
- 6 min read

My friends and family are worried about me as San Francisco Mayor London Breed has now halted the reopening of our city’s businesses because—she says—Covid-19 cases are rising rapidly.
We had not gotten very far in the reopening process: a few restaurants where you could get an outdoor table with a view of boarded shop windows and homeless tents, but it was a step. A step too far, it seems.
San Francisco is a test case of the difficult choices that US cities, counties and states now face, and Mayor Breed says that “our reopening process is guided by data and science”, so let’s take a look at the data.
New cases have been rising since June 15, and the 7-day average has climbed from 23 cases on June 14 to 43 cases on June 23. The Mayor noted June 15 was when the city allowed some reopening of outdoor dining and retail shopping. The virus' incubation period is thought to be 2-14 days, with a median of 5 days. In this case it seems to have been instantaneous, as there was a spike already on June 15 itself: you went out for lunch, got sick, got tested. Go figure.

The rise in new cases is not all due to more testing; the positivity rate (new cases / new tests) has picked up from about 1% to 2.5% on a 7-day average basis. There is a genuine rise in contagion, though the numbers are very small.

In San Francisco, Covid-19 has always mostly infected young people, and the age distribution of new cases is skewing even younger now: people aged under 30 account for over half of new cases in June so far, compared to one-fifth in April; people over the age of 70 account for less of 5% of new cases, compared to 13% in April. The 18-30 bracket has taken the lead in terms of new infections. (In the charts, the numbers on top of each bar are the total number of deaths for the age bracket during the month; on the left axis you can read the share of total monthly deaths; clockwise in chronological order).
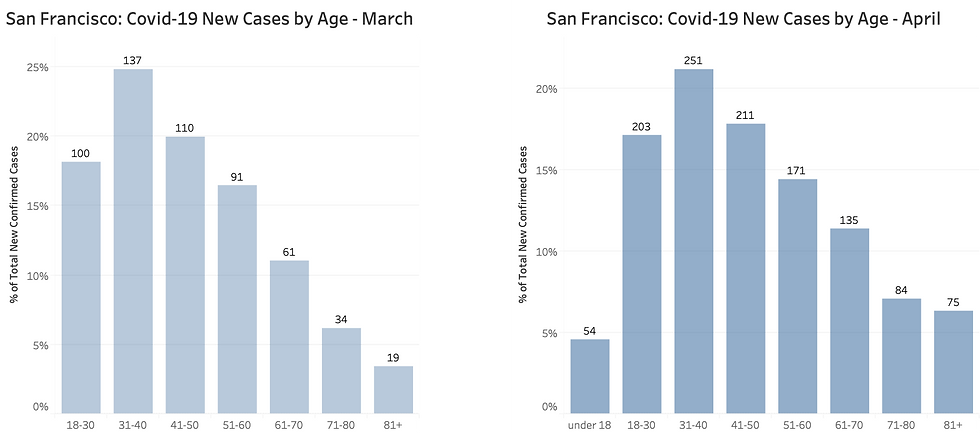
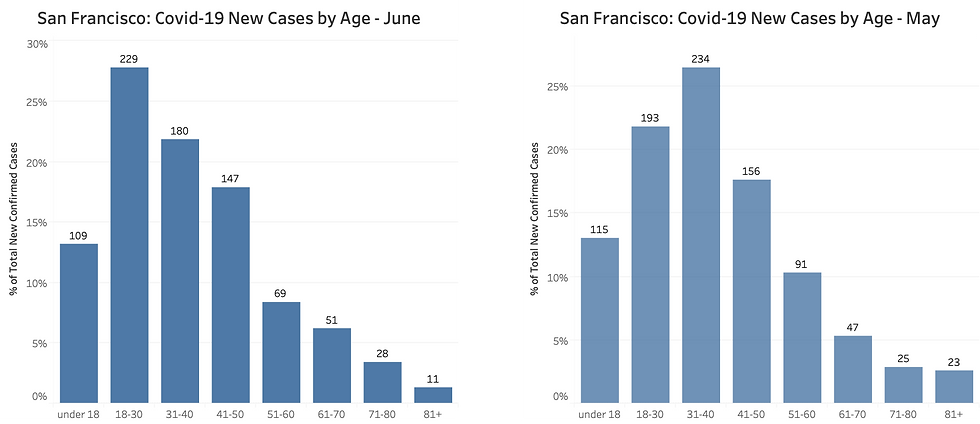
Too many numbers? Here is a simpler snapshot: in April people aged over 60 accounted for 25% of new cases, now less than 11%; people aged under 50 account for over 80% of cases from about 60% in April.

The fact that Covid infections have hit mostly younger people explains why San Francisco has suffered only 48 covid deaths so far. This corresponds to a case fatality rate of just over 1%, and to 53 deaths per million people, which makes San Francisco just a bit more dangerous than Norway, ten times less dangerous than Italy, and fifty times less dangerous than New York City (2,600 deaths per million).

Note also that the spread of infections in San Francisco (3,800 cases per million population) is on a par with Italy (about 3,900); yet the death toll per million population is ten times lower. There are at least two reasons: First, as we have seen, relatively few elderly people have been infected in San Francisco; Second, the Italy-wide data hide the fact that infections were heavily concentrated in some areas of the north, overwhelming the local health care systems. This should be a reminder that focusing attention on the number of new cases does not tell us how dangerous the situation is.
Since the number of elderly people infected has declined, new deaths will likely remain very low and the case fatality rate will decline further; provided of course hospitals don’t become over-burdened. This does not seem likely:
As of June 25, we had 70 confirmed and suspected Covid-19 cases in San Francisco hospitals; this is about half as many as we had in the first half of April.
The number of Covid-19 patients in intensive care has risen from 8 on June 15 to 24 on June 25; compared to these 16 additional patients, there are close to another 400 intensive care beds available (including “surge” beds, which the San Francisco health service defines as “additional beds available to handle an influx of Covid-19 patients.) Covid-19 patients in acute care have risen from 36 to 46 over the same period; compared to these 10 additional patients, there are another 800 beds available, including surge capacity.
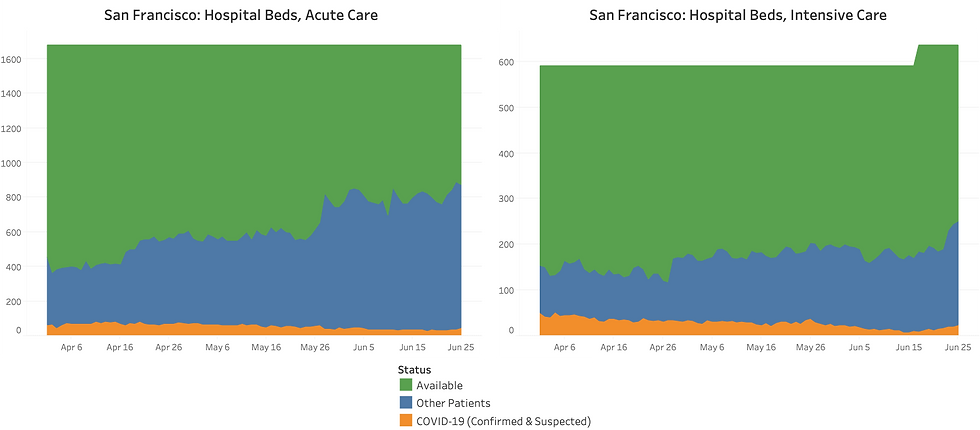
Overall therefore, we have over 1,200 hospital beds available. Less than the 1,700 we had in early April, because we now have more non-Covid patients. But it's still ten times the highest number of hospitalized covid-19 patients seen so far--it peaked at 121 in April.
Where does this leave us?
My view of the data is: yes, new cases are rising, but the absolute numbers are still small (around 40-50 per day); most are young, and therefore less at risk of serious health consequences; there is no evidence so far of rising infections among the older population. Hospitalizations have increased, but again we are talking about very small numbers, there is ample excess capacity in the health care system, and throughout this pandemic we have never even gotten close to reaching capacity.
An increase in infections as we gradually reopen businesses was to be expected—otherwise, the lockdown would have been unnecessary in the first place.
So if it were up to me, I would have kept the already very cautious reopening timetable in place, renewed recommendations to wear masks in public, and kept a close eye on the hospitalizations. I would have intensified testing in the care homes, and urged anyone who needs or wants to have frequent contact with the elderly to be extra careful.
Mayor Breed decided to play it safer. Her concern seems to be that infections might accelerate exponentially, at which point pressure on hospitals could increase rapidly and it might become harder to protect the elderly. So she is halting the reopening—though for now at least she is not imposing new restrictions.
This will have two costs, however: First, businesses will continue to lose money, and more businesses will have to close. Second, people will grow increasingly impatient, and the desire to “throw off the mask” will increase. The rise in infections among the younger cohorts probably reflects their understandable desire to go back to some semblance of normal life – this needs to be managed, it cannot be suppressed indefinitely.
If the Mayor thinks that even the current minor uptick in infections and hospitalizations represents an unacceptable risk, she should tell the city that we will have to live with the current level of restrictions for the foreseeable future. There is still no vaccine or cure in sight, and the virus does not seem inclined to magically disappear by itself. If the policy choice is that we will have to live in isolation for several years, so be it; if hair salons, gyms and restaurants with no outdoor seating have no hope of reopening, their owners and furloughed employees have a right to know.
Across the country (and elsewhere around the world), this is the choice we face. City by city, state by state, we should assess the rise in infections, the age distribution, and the risk in terms of hospital capacity and new deaths. Then policymakers should be transparent about what risk they are comfortable with, and what price they are willing to impose on us in terms of personal and economic restrictions. We are mature enough to get the message and reorganize our lives accordingly.
What policymakers should not do is act as if this rise in cases is a shocking surprise, act as if only the number of new cases matters, and as if the only available response is going back to the same restrictions.
If a reopening process “driven by data and science” means that we are not willing to proceed with the reopening even with the kind of numbers we are seeing in San Francisco, then we will never reopen until a vaccine is found—and it will most likely take a few years. It’s a perfectly legitimate choice—at both local and national level—but we should take it with our eyes open, we should acknowledge and accept the health and economic consequences, and plan for it.
Finally, the message to my friends and family: In San Francisco we are ok, really—don’t worry about me. In fact, if you are not scared of traveling to Norway, you should come visit San Francisco. Oh, right—the travel restrictions…that’s a story for another post.
Comments